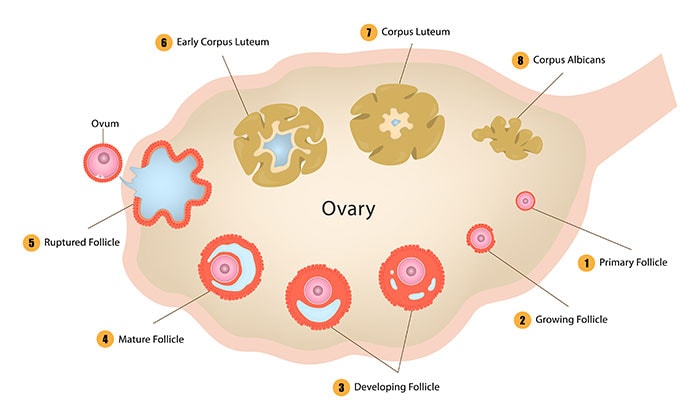
When you hit puberty, your ovaries contain 300,000 to 400,000 follicles. You may be familiar with hair follicles, which are responsible for growing your hair. Your ovarian follicles are responsible for producing estrogen, testosterone, and progesterone as well as immature eggs (oocytes) that may one day become viable human eggs.
But unlike hair follicles, ovarian follicles don’t grow back if they’re lost or damaged. And this is where an artificial ovary could be a gamechanger for couples everywhere.

What causes damage to ovarian folicles?
Endometriosis and cancer treatments are two common causes of damage to these follicles, negatively impacting fertility and hormone production. Plus, as we age, these follicles naturally “die,” decreasing egg and hormone production until we enter menopause.
Cancer fertility preservation
Ovaries and their egg-making follicles are very vulnerable to chemotherapy and radiotherapy treatment. For cancer patients who undergo treatment before puberty, losing these hormone-producing cells messes up the body’s development.
Traditional fertility preservation techniques such as embryo cryopreservation or freezing mature eggs are insufficient for patients who lose ovary function before their eggs mature. Freezing ovarian tissue for cancer patients poses a risk of reintroducing malignant cells.
Currently, hormone replacement therapy (HRT) can solve the loss of hormones after follicle death. But it comes with side effects and risks of its own. In vitro fertilization (IVF) offers a potential fertility solution, along with possible egg donation.
Endometriosis and infertility
Endometriosis affects about 10% of Americans with uteruses. Due to an abnormality, endometrial tissue (the lining of the uterus) spreads beyond the uterus to other parts of the pelvis, such as the fallopian tubes, ovaries, or bladder.
Endometriosis can result in difficulty conceiving. But endometriosis treatment (especially if endometrial tissue has spread to the ovaries) can damage ovarian follicles.
Synthetic ovary development
In 2016, Christiani Amorim at the Catholic University of Louvain in Belgium published a study on the development of synthetic ovaries. The research team took human ovary follicles and implanted them into bundles of fibrin – the protein that forms blood clots.
The team implanted the synthetic ovaries into the abdominal cavities of mice. A week after implantation, over a fifth of the human ovarian cells were still alive. That’s the same percentage of follicles that survive when women receive implants of frozen ovarian tissue as part of existing fertility treatments.
Amorim’s plan for this technology is to help women with endometriosis or those undergoing cancer treatments conceive, or even to delay menopause.
Could an artificial ovary be an infertility treatment option?
That’s the hope! Before undergoing chemotherapy, one ovary would be removed and the follicles placed into a fibrin framework creating an “artificial ovary.” Once the cancer is cleared, the new ovary can be transplanted back to the patient without fear of reintroducing cancerous cells.
For those with infertility caused by endometriosis, donated human follicles could be built into an artificial ovary, then implanted to boost fertility.
According to the American Society for Reproductive Medicine, 6% of married women in the US are infertile. In some cases, an artificial ovary could restore fertility and the ability to naturally conceive.
Artificial ovary for delaying menopause?
Because the ovarian follicles release important hormones like estrogen, implantation of an artificial ovary would essentially “refill” the body’s naturally declining hormone production. Reintroducing estrogen production and ovulation would allow patients to delay menopause (and its difficult side effects) and extend a woman’s childbearing years.
The average age of menopause in the US is 51. Fertility starts declining at age 30 and once you hit 35 the chance of pregnancy complications increases. The average age for first-time mothers in the US is now 26 (31 in other developed countries.) More and more people are delaying having children, but our bodies haven’t gotten the memo.
While there are many assistive reproductive technologies, wouldn’t it be great if ovarian function could be restored or extended instead of going through assisted or artificial conception?
The future of the artificial ovary
While the artificial ovary has not yet been approved for human use, a research team from Rigshospitalet in Copenhagen presented their working bio-engineered ovary at the European Society of Human Reproduction and Embryology annual meeting in 2018. We don’t have news of successful human trials yet, but we’re keeping our eyes peeled for future developments!
About The Outpatient Hysterectomy Center
As two of the nation’s leading obstetrics and gynecology surgeons, Drs. Thaïs Aliabadi and Ramon Yera offer the very best in women’s health care. Together with their warm professional team, they create a special one-on-one relationship between patient and doctor.
We invite you to establish care with the Outpatient Hysterectomy Center. Please click here to make an appointment or call us at (844) 863-6700.
The Outpatient Hysterectomy Center is conveniently located to patients residing throughout Southern California and the Los Angeles area. At the Cedars-Sinai Medical Center, we are near Beverly Hills, West Hollywood, Santa Monica, West Los Angeles, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles, to name a few.