Do you have questions about laparoscopic and robotic surgeries?

With all of the technological developments in medicine today, it’s hard for the layperson to keep up. This isn’t made easier by advertising from medical device companies and hospitals peddling their new-fangled devices, making it hard for the average person to determine whether a new technology may be suitable for them.
I thought I’d try to dispel some of the confusion by answering questions that patients often ask me about the differences between laparoscopic and robotic surgery.
Is laparoscopic surgery the same as robotic surgery?
Not at all. Let me explain some of the differences.
What is laparoscopic surgery?
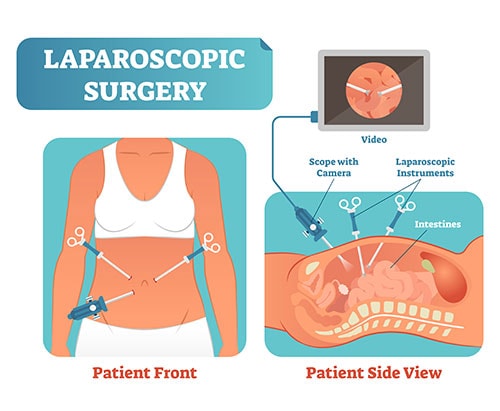
Laparoscopic surgeries are out-patient minimally invasive surgeries that allow the surgeon to see your pelvic organs through a laparoscope – a thin flexible tube with a lighted lens at the end. This allows them to see, for example, your uterus, fallopian tubes, ovaries, endometrial tissue, bowel, and bladder.
Laparoscopes for pelvic surgery can be fitted with tools to perform highly specialized surgical tasks such as removing polyps or tumors or taking tissue biopsies. These are manual tools that allow the surgeon to feel the tissues on the end of the instrument, providing tactile feedback during surgery. This is important when it comes to avoiding injuring nearby organs, nerves, and blood vessels.

Conventional laparoscopy is widely used in obstetric and gynecologic surgery to diagnose and treat conditions such as uterine endometriosis.
At our practice, we specialize in advanced minimally invasive laparoscopic surgery developed through years of practice. We’ve performed thousands of procedures, including removing watermelon-sized fibroids and performing a total hysterectomy (removal of the uterus) through a few tiny abdominal incisions. The end result is virtually no pain, no complications, minimal bleeding, and a quick recovery. What’s more, our techniques reduce the risk of spreading cancerous cells throughout the pelvis during surgery to almost nil.
What is robotic surgery?
With robotic surgery, the surgeon sits at a computer console and controls the movement of robotic arms, one of which holds a camera transmitting live video images that help the surgeon guide the robot. Other arms have surgical tools that are computer-controlled to perform specific tasks. The manufacturer claims that the surgical robot was designed to help overcome some of the limitations that come with a laparoscopy or laparotomy.
Many patients have heard of one of the more famous robotic surgical systems: the DaVinci system made by Intuitive Surgical. DaVinci’s advertising claims that the robotic 360-degree visualization of the surgical field offers an advantage in invasive surgical procedures.
Precise control of the robotic arm depends on both human and device factors:
- Having a surgeon with a very high degree of experience with this technology (which is not taught during medical training)
- And accurate data transmission between the surgeon’s console and the robotic surgery arm
Robotic vs. Laparoscopic Surgery for Hysterectomy & Pelvic Procedures
It depends. When performed by highly experienced surgeons, robotic surgery can be better than traditional open surgery for specific types of procedures. For example, in urology, robotic surgery is used for prostate removal (prostatectomy) to treat cancer. According to an article in Nature, by 2014 nearly 90% of prostate removals were done robotically. Robotics are also effective for hernia repairs and gallbladder resections.
Manufacturers claim robotic surgery advantages include lower complication rates for perioperative pain, blood loss, scarring, and infection occurrence; plus shorter hospital stays when compared to traditional open surgery. However, after reviewing several years of surgical outcomes, the FDA published a warning in 2019 stating the safety and effectiveness of robots have not been established for performing procedures that prevent and treat cancer.
What are the risks of using robots in surgery?
Because robotic surgery requires extensive training and many surgical hours to gain proficiency and dexterity controlling the robot arms, there can be operator error risk in addition to the inherent risk of complications due to malfunction of the device itself.
Most people would be surprised to learn that there are no national training standards for robotic surgery. In fact, the training typically consists of just one-day hands-on sessions at the manufacturer’s headquarters, some online instruction, and two supervised surgeries. There’s a very steep learning curve to climb to master surgical techniques using robotic assistance; it takes many dozens, if not hundreds, of surgeries to achieve proficiency using a robot.
The most commonly reported short-term complications of robotic surgery are due to hemorrhage caused by lacerations of organs or blood vessels during dissection. Other complications include inadvertent injury to surrounding tissues, nerve damage due to pressure from fixed patient positioning during a long surgery, and even blindness.
It’s also important to remember that a surgical robot, like any mechanical or electronic device, can be subject to loss of calibration or even failure over time.
The simple truth is that most major hospitals in large metropolitan areas have a robot “on staff” in order to remain competitive in today’s technology-driven medical environment. Because these machines are very expensive to purchase and maintain, surgeons are encouraged to use them to help defray their cost. Unfortunately, this may lead to more robotic surgery being recommended than is warranted.
Is robotic surgery better than our advanced laparoscopic surgery for pelvic procedures?
In my opinion, no. When it comes to gynecologic surgery, our advanced laparoscopic approach is far superior to the robotic approach. A retrospective meta-analysis study published in the Journal of the American Medical Association did a systematic review of more than 250,000 hysterectomies and found that clinical outcomes for robotic surgery for hysterectomy were no better than for laparoscopic surgery during follow-up.
The only significant difference was that the robotic hysterectomy was more expensive and the operative time was considerably longer. So, if robotic surgery doesn’t out-perform conventional laparoscopic surgery, it begs the question “then why is it performed so often?” One possible explanation might be that the ergonomics involved in performing surgery by operating a joystick seated at a computer console in an operating room are way better for the surgeon than standing at the operating table.
In over 20 years of performing advanced laparoscopic surgery, Dr. Yera and I have found that laparoscopies involve notably less operating time (meaning less time under anesthesia) than robotic procedures and the medical literature bears this out. It has also been our experience that laparoscopies involve less intraoperative blood loss than either traditional or robotic surgery, less postoperative pain, quicker recovery time, nearly zero postoperative complications, and a much lower risk of infection. All this with the advantage of no overnight hospitalization.
But most importantly, when there’s a chance of cancer being present, our advanced oncology surgical techniques are optimal. They reduce the risk of spreading cancer cells throughout the abdomen by containing the tumor tissue in a bag before removing it from the body.
Is everyone a candidate for laparoscopic surgery?
Pretty much every patient requiring pelvic surgery can undergo a laparoscopic procedure. That’s because it’s way less invasive than an open procedure and involves less time and, in some ways, less risk than robotic surgery. That said, the only real way to determine whether you can benefit from a laparoscopic procedure is by coming in for an examination and consultation. During your consultation, we can discuss your health concerns and come up with a treatment plan that takes your health and quality of life into consideration.
If you are considering having gynecology surgery, it is very important to discuss any concerns you may have with your healthcare provider.
About The Outpatient Hysterectomy Center
As two of the nation’s leading gynecological surgeons, Drs. Thaïs Aliabadi and Ramon Yera offer the very best in women’s surgical care. Together with their warm professional team, they create a special one-on-one relationship between patient and doctor.
We invite you to establish care with the Outpatient Hysterectomy Center. Please click here to make an appointment or call us at (844) 863-6700.
The Outpatient Hysterectomy Center is conveniently located to patients residing throughout Southern California and the Los Angeles area. At the Cedars-Sinai Medical Center, we are near Beverly Hills, West Hollywood, Santa Monica, West Los Angeles, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles, to name a few.
Sources
Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014; 123 (1):5–12. doi: 10.1097/AOG.0000000000000006. [PMC free article] [PubMed]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4854942/
Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol. 2014; 66 (2):303–318. doi: 10.1016/j.eururo.2014.02.053. [PubMed]
https://pubmed.ncbi.nlm.nih.gov/24631406/
Randomized clinical trial of standard laparoscopic versus robot-assisted laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2006 Nov;93(11):1351-9. doi: 10.1002/bjs.5535.
https://pubmed.ncbi.nlm.nih.gov/17058295/
Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol. 2009;16:1480-87.
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S2237-93632019000400351